Plantar Fasciitis

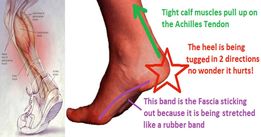
One of the most common causes of heel pain is plantar fasciitis, caused by inflammation of the thick fibrous fascia that runs along the sole of the foot, connecting the heel bone to the toes (plantar fascia)
CAUSES:-
The plantar fascia acts as a shock-absorber to the arch of the foot and too much tension will result in small tears in the fascia. Repetitive tearing can cause inflammation and consequently pain.
• sudden stretching or overuse of the sole of the foot eg. sprinting, jumping and landing on hard surfaces or after increasing running distance/ intensity
RISK FACTORS:-
• Age - most common between the ages of 40 and 60
• Overuse /certain types exercise - stress on your heel and attached tissue eg. long-distance running, ballistic jumping activities, ballet dancing and aerobic dance
• Foot mechanics - flat feet/having a high arch(pes cavus)/abnormal gait can affect weight distribution when standing and increase stress on the fascia
• Obesity - extra weight may put extra stress on the fascia
• Occupation – standing on your feet for prolonged periods eg. factory workers, hairdressers
• tight calf muscles – pulls on the heel away from the plantar fascia
• Poor cushioning/arch support in your shoes
SYMPTOMS:-
• stabbing pain in the sole of the foot near the heel or the arch of the foot
• pain usually worse when first standing in the morning/ prolonged standing/ rising from sitting
• pain usually worse after exercise, not during
• usually gradual onset of pain
• walking short distances may improve pain, longer distances may increase pain
• Pain with sudden stretching of the sole of the foot eg standing on toes, walking upstairs
• Pain worse when wearing flat or unsupportive footwear

TREATMENT:-
Plantar fasciitis usually resolves itself but the following can minimise symptoms: -
• avoid activities that make the pain worse • avoid walking barefoot on hard surfaces
• The RICE method – REST for a few days, ICE for 15-20 min periods, COMPRESS with a support bandage, ELEVATE
• Anti-inflammatories eg ibuprofen
• Wear shoes with cushioned heels and good arch support, using insoles if needed
• exercise may improve symptoms so even if on rest from a particular activity, you should maintain gentle walking
• if symptoms persist past 4-6 weeks, seek advice from physiotherapist / GP /podiatrist
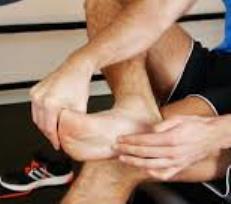
• Massage – massage focused on the arch of the foot and surrounding muscles may offer relief, massage of the calf muscles may also help if these are tight
• Physiotherapy and cortisone injections if symptoms persist
STRETCHES:-
Stretching can reduce tension in the foot and calf, reducing pain and a steadily improving symptoms over time.
• Calf stretches - standing against a wall

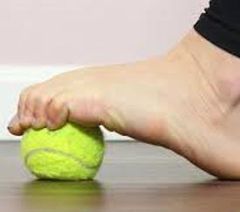
• Rolling stretch –rolling a ball forwards and backwards under the sole of the foot

• Stretching the plantar fascia – with affected foot resting on other leg, pull the toes toward the shin to create tension in the arch of the foot
• Foot flexes – increases blood flow and relieves tightness in the calf

• Toe curls – can be done using a ball,or by using the toes to grasp the centre of a towel on the floor if easier While the foot exercises can be helpful, it is recognised among orthopaedic specialists that stretching the calf muscles can give more improvement.
OUTLOOK:-
Plantar fasciitis may cause chronic heel pain, making regular activities difficult, if not treated. Changing your walking pattern to compensate for the pain may result in issues with the feet, knees, hips or back.
