- 07736 104738
- sam@medicalmassagelady.com
- Mon - Sat, 8:00 - 18:30
A stroke (CVA-cardiovascular accident) can appear to be a very sudden occurrence, potentially leaving someone unable to move, speak or communicate. They occur as a result of reduced blood flow in the brain, which prevents oxygenation and nutrition of the brain tissue, and therefore can cause brain damage or death.
There are three main types of stroke:-
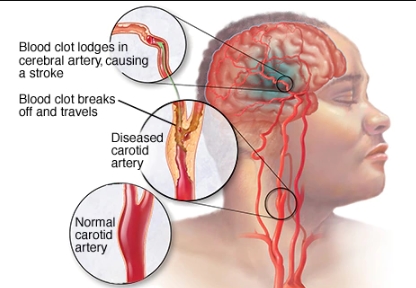
- Ischaemic stroke – this is the most common, caused by a clot cutting off the blood supply to the brain.

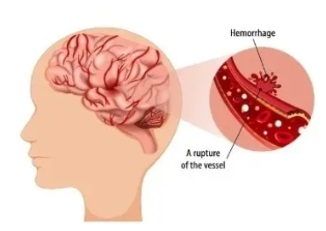
- A Haemorrhagic stroke is caused by bleeding in or around the brain.
- A transient ischaemic attack or TIA is also known as a mini-stroke. It is the same as a stroke, except that the symptoms last no longer than 24 hours.
The risk of a second, more severe stroke following a TIA is highly likely, so lifestyle factors (including daily diet and exercise) to reduce the risk should be assessed.
In the UK, strokes are a major health problem, with around 110,000 occurring per year, making them the third largest cause of death, after heart disease and cancer. Stroke induced brain injuries are also a leading cause of adult disability in the UK.
Approximately one in eight people die within 30 days of having a stroke, so urgent medical care is a priority to minimise the damage. The aftermath is different for everyone, but the physiological and psychological changes that occur, can cause a deep sense of loneliness. There may be some paralysis, weakness of muscles, difficulty with speech or memory loss.
There are two stages of treatment after diagnosis: acute care and post-acute or chronic care. Massage therapy is not recommended in the acute stage due to the circulatory problems likely to be present, but it can be an integral part of post-acute care, having a positive impact on both paralysis and muscle weakness. Neuro-massage is an important part of stroke treatment, helping to improve nerve function and joint mobility, and ease stress associated with the trauma of having had a stroke. As massage practitioners we may be asked to treat someone who has had a stroke and we should know what we are dealing with before we decide how to treat someone – and importantly whether or not we should treat someone at all.
RISK FACTORS
The incidence of strokes is higher in:-
- Older people
- South Asian, African or Caribbean(due to a predisposition for high blood pressure)
Smoking - Overweight
- lack of exercise
- too much alcohol and a poor diet
- high cholesterol
- atrial fibrillation
- diabetes
- high blood pressure
- family history
CAUSES
- Blockages caused by a blood clot developing within brain vessels or emboli that travel from a distant site to lodge into brain vessels (ischaemic)

- bleeding within the brain (haemorrhagic)
- cause unknown (cryptogenic)
SYMPTOMS
The immediate symptoms of stroke can be remembered with the word FAST: Face-Arms-Speech-Time.
Face – the face may have dropped on one side, the person may not be able to smile or their mouth or eye may have dropped. Arms – the person with suspected stroke may not be able to lift both arms and keep them there because of arm weakness or numbness in one arm. Speech – their speech may be slurred or garbled, or the person may not be able to talk at all despite appearing to be awake. Time – it is time to dial 999 immediately if you see any of these signs or symptoms


ask the person to stick their tongue out, if it is crooked or goes to one side, assume it is a stroke
- Paralysis – either flaccid or spastic paralysis.
- FLACCID PARALYSIS means that there is no nerve impulse transmitted down the limbs ie.the muscles receive no signals to move, causing the limb to hang. In arms this can contribute to shoulder strain due to absent shoulder-joint muscle tone. If it is a leg that is affected then it can give problems in the hips and lower back.
- SPASTIC PARALYSIS means that the muscles respond but without control, so the stronger flexors contract, turning the limb inwards. In the long term, this results in shortened tendons and can cause ossification of the joints, particularly in the knee, elbow and wrist. Bone is then effectively laid down in connective tissue, causing fingers and toes to curl tight
COMPLICATIONS
Stroke complications may last a few hours or the rest of an individual’s life
- Sensory damage, including numbness or vision loss
- Confusion, headaches, vomiting
- Motor damage
- Partial or full paralysis of one side of the body
- Paraesthesia- numbness and tingling in affected limbs
- Dystonia - unintentional sustained muscle contractions
- Impaired coordination and proprioception
- Slurred speech or loss of language (aphasia)
- Difficulty understanding written language(alexia)
- Loss of the ability to identify objects (agnosia)
- Difficulty swallowing (dysphagia)
- Memory loss
- Depression
MASSAGE THERAPY FOLLOWING STROKE
While massage therapy won’t be able to reverse the damage caused by the stroke, it may ease some of the symptoms and offer sense of connectivity through the recovery period, as well as providing therapeutic touch when the majority has been more clinical. However, massage can only take place later in the recovery process, alongside other healthcare professionals, eg. physiotherapist, occupational therapist, speech therapist etc. as the complexities of stroke require a more in-depth treatment plan.
There is no typical approach following a stroke, it depends on the type of stroke and the complications that arise, but generally massage therapy should focus on stretching out and soothing muscles that are contracted and tight and bringing awareness to flaccid and paralysed areas.
WHAT THE RESEARCH SAYS
- massage may reduce the effects of constipation in stroke patients
- Ayurvedic-based massage can promote healing in those with flaccid muscles and reduce the need for antispastic drugs
- physical touch eases anxiety in stroke clients and improves sleeping quality
- aromatherapy can reduce stress, have a positive impact on mood and improve sleep in stroke clients
BENEFITS OF MASSAGE
Neuro-massage is particularly beneficial for stroke patients as it is applied in a very gentle and specific way.
Benefits of massage for stroke patients include:-
- IMPROVED SENSATION & INCREASED BODY AWARENESS - helps get used to new sensations in affected parts of the body and to touch in general following the stroke, as well as increasing awareness of flaccid and paralysed limbs and limbs that may be neglected due to visual disturbances
- BOOSTS CIRCULATION - in areas that are immobile, improving skin colour and tone.Massage has been shown to help dilate superficial blood vessels, thus increasing the blood flow to an area, as well as improved lymphatic drainage and reduced swelling. All of these can help improve function and decrease pain related to swelling. Massage must be very gentle, however, so lymphatic drainage is ideal for a stroke client. By improving circulation and regenerating muscle function massage may help repair sensory damage.
- REGENERATED MUSCLE FUNCTION - can address joint stiffness and postural changes and decrease muscle spasticity, thus improve range of motion and help to regain muscle control. Once far along enough in the recovery process to be able to offer deeper work, if not contraindicated, deep tissue massage with some passive stretching can encourage proprioception, by stimulating the nerves and sensory end organs which guide the muscles. By promoting circulation of blood, oxygen and lymph to neglected areas, massage can also improve mobility and detoxification.
- AIDS RELAXATION AND SLEEP
- INCREASED SEROTONIN LEVELS – massage is known to increase serotonin levels, which can alleviate depression. Increased serotonin levels can also reduce the risk of vascular problems as a result of antidepressants, hence potentially also reducing the risk of heart attack or a repeat stroke. Depression is also a risk factor of stroke, so massage could even reduce the risk of stroke prior to a CVA happening
- REDUCED STRESS AND ANXIETY – by inhibiting cortisol release massage therapy also eases stress and anxiety, which may not be a direct result of a stroke, but can occur alongside other physical health issues, so improving overall mental health can encourage healing
- REGAINED MEMORY - reflexology can work on points related to the brain, spine, neck, adrenals, and heart points, potentially assisting with memory loss and communication issues
CONSIDERATIONS FOR MASSAGE TREATMENTS
- Primary focus should be on reducing any swelling with lymphatic drainage to assist the removal of toxins and waste products
- re-educate client movement pattern by improving sensory stimulation. Light touch can help sensory neurons to regain stimulation capabilities
- it is wise to ensure the client can still communicate verbally throughout the session and keep work on the neck to a bare minimum and less intense to reduce blood flow into the brain
- static compression on a muscle can decrease spasticity
- passive stretching can assist with joint stiffness
- gentle range of motion exercises and light myofascial release, skin traction and gentle tapotement may help to increase awareness in the nervous system and work on any adhesions in the tissue
- massage therapists should continue to liaise with other therapists involved
- reflexology or foot massage maybe helpful in clients with clonic ankles (abnormal involuntary muscle contractions)
- if peripheral artery disease (PAD) is an issue, avoid deep, vigorous massage(which shouldn’t be used in stroke clients anyway) to avoid potentially dislodging a clot
- slowing down massage techniques and focusing on one body region may help to reduce the risk of a repeat stroke
- if hypertension is an issue, it is important to check any sensations of dizziness during the massage. Back massage can reduce blood pressure, decrease heart rate and improve parasympathetic activity
CONTRAINDICATIONS
Massage treatment is completely contraindicated certainly within a month of having a stroke, due to the increased risk of having a second stroke, but even in the first 6 months following, there should be no neck massage in case of any clots. The impact of massage on the circulation should always be considered when dealing with a client who has had a cardiovascular incident. Also any massage done during this time should be performed by someone who is qualified and experienced in dealing with strokes, and after consultation with the clients doctor.
It is also important to know that the client’s blood pressure is controlled and to take into account any particular positioning requirements, particularly in the case of flaccid paralysis. Medications will also be a factor in the decision of whether to proceed with a massage treatment, and if so, what type of massage.
Many stroke patients will be taking anticoagulant medication to help prevent another stroke and so are prone to bruising, so any massage must be light rather than deep tissue. In those taking warfarin or heparin, it would also be important to check levels and assess for any bruising prior to starting massage. Common medications include:-
THROMBOLYTICS
- Eminase
- Streptase
- Retavase
ANTICOAGULANT
- Warfarin
- heparin
ANTIPLATELETS – to limit formation of new clots
- Plavix
- Effient
- Aspirin
- Novasen
Antihypertensives (ACE inhibitors, calcium channel blockers) may also be used to stabilise the blood pressure, but there may be side effects which also need to be taken into account, for example, gastrointestinal issues, blurry vision, headaches and fatigue.




